Scientists have found a genetic link and a potentially causal relationship between endometriosis and some types of ovarian cancer.
The absolute risk of an endometriosis patient developing cancer is still very low, but these overlapping genetic markers could help researchers understand and treat both illnesses better in the future.
"We don't want women with endometriosis to worry, but rather we want them to be aware and know that the purpose of this study was to increase our understanding of both of these diseases by understanding the genetic link between them," explains molecular bioscientist Sally Mortlock, from the University of Queensland, Australia.
Endometriosis is a highly common and notoriously underdiagnosed condition. It occurs when cells similar to the lining of the uterus grow elsewhere in the body, sometimes causing pain or infertility.
Similar to other female pain conditions, endometriosis, or 'endo' for short, has been historically overlooked by medicine, and thanks to that setback, today, we still know very little about it, including how it's caused.
Recent research suggests endo holds a strong genetic component, often clustering in families. Epidemiological studies have also shown those with endo are more likely to develop ovarian cancers later in life.
To further investigate the relationship between these two conditions, researchers in Australia gathered together data from several genome-wide association studies.
In the end, they found 19 genetic locations in female DNA that appear to predispose people to endo while also predisposing them to epithelial ovarian cancer (which is the kind that develops in the lining outside the ovary).
"Overall, studies have estimated that 1 in 76 women are at risk of developing ovarian cancer in their lifetime, and having endometriosis increases this slightly to 1 in 55," says Mortlock.
We still don't know how to predict which endo patients are more likely to develop ovarian cancers, but Mortlock's recent research gives us a few clues.
The study used genomic data from several large and recent meta-analyses on endometriosis and epithelial ovarian cancer. Unlike previous studies, however, the authors were able to causally associate the genetic components of endometriosis with some types of ovarian cancer.
In simple terms, this means researchers found the genes responsible for endometriosis were driving the development of tissue that increase the risk of developing ovarian cancer, but not the other way around.
This directionality suggests that endometriosis and epithelial ovarian cancer (EOC) are biologically related, and that "a genetic variant's effect on endometriosis is likely to cause its effect on EOC for the variants highlighted in this study", according to the authors.
The genetic regions shared by endometriosis and EOC could help experts figure out what mechanisms are driving this causal relationship and what biological pathways might contribute to the risk.
Such research could provide potential drug targets and treatment options for both illnesses, halting their progression.
In the current study, for instance, some shared genetic variants were found in regions known to host hormone-responsive genes.
This suggests hormone regulation might help block the causal pathway between endometriosis and a type of EOC known as clear cell ovarian cancer (CCOC), which is associated with abnormal tissue growth outside the uterus.
The authors also note that cell adhesion pathways were "significantly enriched" for some genetic variations shared between endo and CCOC. This suggests the ability of endometriosis lesions to adhere to tissue might be an important part of disease development for both illnesses.
Endometrioid ovarian cancer (ENOC) was also similarly associated with endometriosis, and, to a lesser extent, high-grade serous ovarian cancer (HGSOC), which is one of the deadliest human cancers with few predictive biomarkers.
Some of the genetic markers for endo and EOC identified in the current study are also shared with other reproductive diseases, like polycystic ovary syndrome and uterine fibroids.
The authors, therefore, suspect the "perturbation of underlying pathways important for the development and regulation of the reproductive and endocrine systems may predispose women to a variety of diseases", depending on their genetic and environmental risk factors.
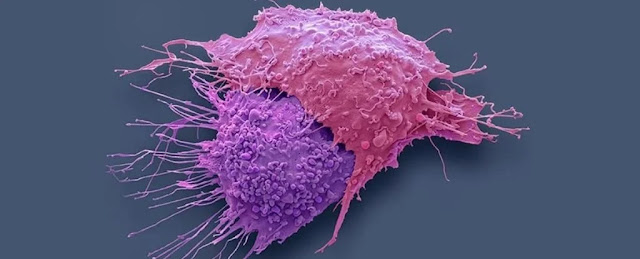
Endometriosis itself is not cancerous, but over the years, researchers have compared the way endometrial lesions metastasize, spread, invade and damage tissue to that of cancerous cells.
Some case studies have even shown that on very rare occasions, endometrial lesions can transform into malignant tissue.
There are still so many avenues to explore when it comes to understanding endometriosis, but genetic studies like these can help experts whittle down the numerous options in front of them, pushing future research in the right direction.






No comments:
Post a Comment